
Pay special attention to aging claims, those that aren’t being processed within the typical timeframe. You may need to prompt a clearinghouse or payer to identify why it’s stalled and how soon it can be resolved. E&M codes are a subset of CPT codes used to document and bill for patient encounters, including initial assessments, follow-up visits, and consultations. Mental health professionals use E&M codes to indicate the complexity and level of service provided during an appointment.
- These capabilities can significantly reduce denial rates and accelerate reimbursement cycles.
- Use your reference ID from your eligibility and benefits verification phone call to fight your case.
- By following these insights, you’ll traverse the landscape of mental health billing with confidence, ensuring that financial procedures align seamlessly with the quality of care extended.
- If your claims require appeal, speak to a customer support representative about obtaining the necessary forms to file your appeal.
- This process entails intricate procedures, coding precision, and meticulous documentation, all aimed at facilitating reimbursements from insurance providers.
High Denial Rates
- Happy to do this whole process for you as every other billing service should.
- CPT codes are a standardized set of codes maintained by the American Medical Association (AMA).
- In other words, if you’re wondering if there are ways to improve your billing processes and increase the revenue for your mental health organization, there’s hope.
- ICANotes is the premier EHR for behavioral health specialty, and we work with all clinical disciplines to deliver an intuitive charting solution for your practice.
- Gathering the information from your clients is only the first step, it’s also your responsibility to ensure that it’s accurate, up-to-date and eligible.
Mastering mental health billing is pivotal for seamless access to quality care while maintaining financial equilibrium. By Accounting Periods and Methods decoding the intricacies of insurance, coding precision, and efficient claims processing, mental health practitioners bolster their ability to provide essential services. This guide illuminates the path toward harmonizing compassionate mental health support with the pragmatic demands of financial processes. At the heart of mental health billing is the use of accurate CPT (Current Procedural Terminology) codes.
A Complete Guide to Mental Health Billing
- One survey found that about one in five insured adults who used mental health services (22%) say they had a denied claim.
- By adopting these strategies, mental health practitioners can simplify their billing processes, ensuring they remain focused on what truly matters—providing quality care to their patients.
- If they don’t have insurance, you’ll need to try to get payment from the client.
- When considering whether to join a network or accept payment from insurers, it’s important to evaluate their pre-approval rules and their limits for payment.
- When you start working for a new client, always check if preauthorization is required before providing any non-standard session.
Also perform a new eligibility and benefits check for that client from Chapter 2 of this mental health billing for dummies guide. Make sure you’re filing claims to the right place, with the right information. Behavioral health services often involve many types of treatment options and medication management, each with different billing codes and insurance policies. For example, one report found that mental health visits are six times mental health billing for dummies more likely to be out-of-network than primary or specialty care. Another effective strategy is outsourcing billing tasks to a professional billing service that specializes in mental health.
How to Check Eligibility and Benefits for Mental Health
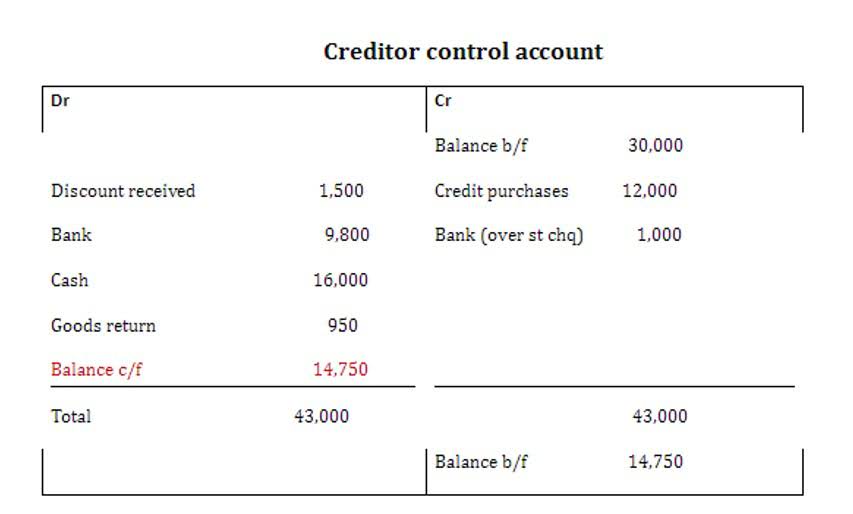
Monitoring the status of your claims is crucial; follow up on any denials or requests for additional information promptly to resolve issues and ensure timely reimbursement. In essence, while mental health billing and behavioral health billing share similarities, the latter encompasses a broader array of psychological services. Understanding their relationship is vital for practitioners, insurers, and policymakers working to improve access to comprehensive mental and emotional well-being care. Explore the core elements of mental health billing and master best practices for precise coding and documentation, empowering practitioners and stakeholders alike.
- Behavioral health billing and coding is the process of accurately documenting, submitting, and obtaining reimbursement for mental health and substance abuse treatment services.
- So, although you’re technically submitting your claims electronically in this sense, it’s STILL a very manual process.
- Your access portal for updated claims and reports is secured via our HTTPS/SSL/TLS secured server.
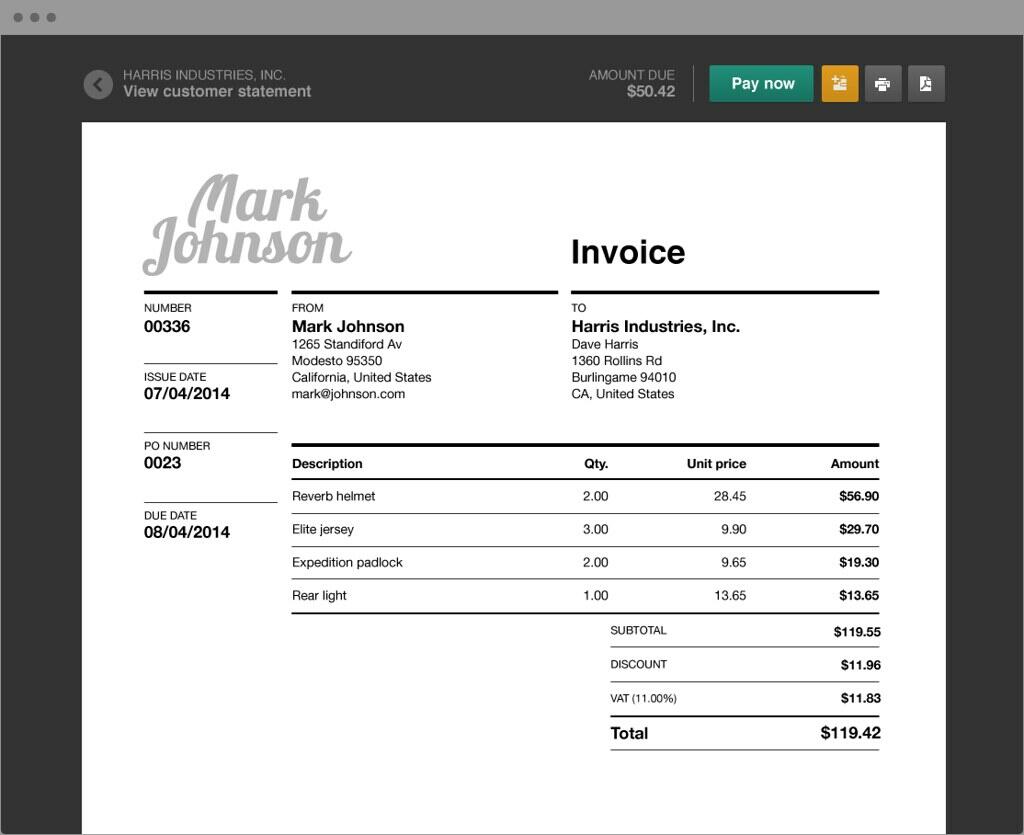
- After this process, you have all of the information required to file claims, what to charge your client when they come in for a visit and how to file their claim via online or otherwise.
- If ALL of your patients had Health First Colorado as their payer, this wouldn’t be that bad of a manual process…but that’s not the case.
- If insurance refused to cover the entire cost of services, you’ll have to bill your patient for the difference.
If you are struggling to find out the place of service code or modifier to use for your insurance claims, this is something we provide as part of our billing service free of charge. The majority of group practices and almost all successful individual private practices utilize outside billing services in one capacity or another. If the claim has not been received, no corrected claim needs to be submitted, the original claim needs to be submitted. Ensure you refile claims in a prompt manner to make the timely filing window for claims submission. Call the same company using the same eligibility and benefits number and ask for claims processing and EOB accounting.

Health insurance organizations don’t make this entire process easy, but they have their rules. The unique payers that still cling on to paper stand no chance against the most ideal alternative for claims processing. Your clearinghouse’s sole purpose is to “have your back” when it comes to mental health billing. When these payers present themselves, it’s not the end of the world but it does present a process change.

Bir Yorum Yazın